Private providers
Support in managing the end-to-end mental health care pathway across multiple geographic sites.
Targeted support
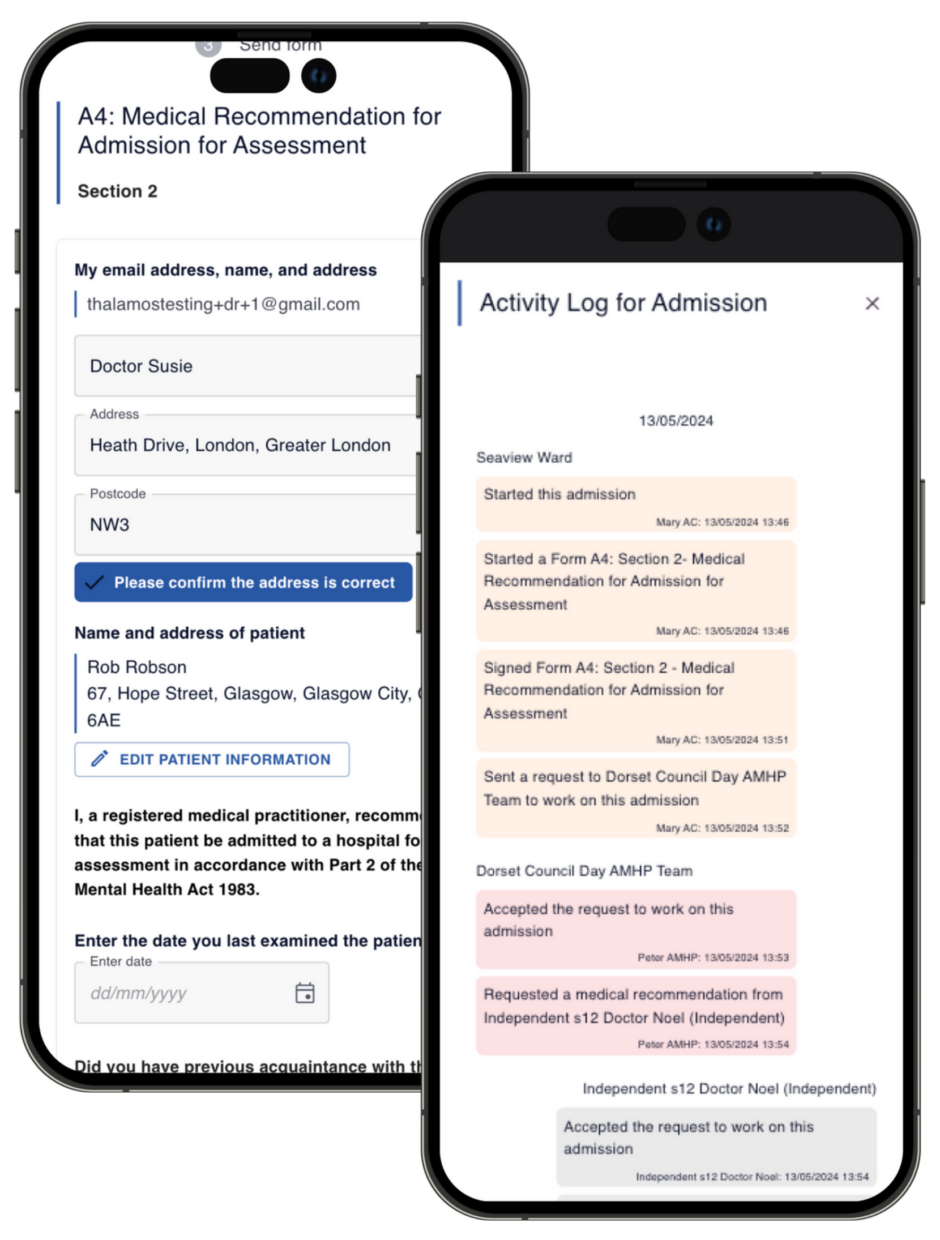
Thalamos eMHA in private mental health care settings fully demonstrates the breadth and flexibility of functionality provided within the software and the workflow processes it creates.
Thalamos enables private care providers to manage the end-to-end mental health care pathway across all their geographical sites, delivering true oversight of MHA performance with partner health and care organisations.
By both centralising and devolving MHA processes within local teams, Thalamos eMHA provides a fully compliant, traceable, and auditable Mental Health Act trail to better inform single site operational decisions as well as driving efficiencies across all provider sites.
Benefits
- Interoperable readiness
- Time saving on administration
- Protection for patients and their data
- Patient outcomes and treatment times
- Administrative and clinical time savings to support improved patient care, staff training and improved services
- Clinical safety and compliance
- Simpler information governance
- Compliance, creating best practice
- Operational efficiency
- Standardisation
- Supporting workflows with partner organisations
Case Study

Cygnet Health Care
In 2021 Thalamos were commissioned to deliver a Mental Health Act (MHA) digitisation programme across Cygnet’s 58 mental health hospitals in England, including MHA and clinical teams, and with local AMHP teams and NHS providers.
What we delivered
The Cygnet implementation involved deploying 58 MHA team portals and digitising their local ecosystems of users and pathways. This was particularly challenging with Cygnet due to the quantity, and geographic spread of hospitals with functionality requiring deployment across 58 local ecosystems and insights required between the nationally distributed sites.
How we successfully achieved this
Delivering against such an ambitious programme of work across many dispersed national sites required a carefully considered four-phase deployment that adhered to a robust implementation plan, documenting milestones, risks, and KPIs. The key inherent risks for such a large implementation were mitigated by:
- Mapping local ecosystems across 58 sites
- Engaging all stakeholders, Cygnet & 3rd party (AMHP Teams)
- Co-ordinating resources to deploy nationally

The four-phase deployment included:
- Programme establishment and kick off
- Process mapping and stakeholder engagement
- Orientation/training
- Roll-out/adoption
The Cygnet roll-out commenced on 15 March 2021, with an agreed target of 80% of users trained within one month.
By 20 April 2021, 87% of users were successfully trained.
Patient benefit
Thalamos has helped reduce access to treatment times from 7 days to 15 hours by connecting care professionals more effectively.
Clinical benefit
With forms incapable of getting lost on Thalamos, this supports private provider multi-agency working as well as time saved for staff.
Compliance benefit
At one site using paper, there was an estimated 25% error rate. This error rate has been dramatically reduced to 1.6% since using Thalamos.
We believe that there should be no distinction or disparity between emergency physical and mental health care as exists currently.